
Whether you're a private practice or a large healthcare facility, insurance credentialing is a vital step in launching your new revenue cycle. Unfortunately, even if you know which insurance companies you want to collaborate with, the credentialing process can be both time-consuming and frustrating. This is why many healthcare organizations opt to outsource this critical task.
At Ambit, we're committed to being your trusted Practice Management Concierge. We handle insurance credentialing for physicians, hospitals, and a variety of other healthcare institutions. From beginning to end, we’ll walk you through every step of gaining approval from insurance payers. Discover why so many healthcare professionals and organizations rely on us for their medical insurance credentialing services.
In today's healthcare environment, accepting patients' insurance plans is key to your practice's success. Health insurance credentialing, also known as provider insurance credentialing, is the process medical insurance companies use to evaluate your application for inclusion in their provider panels. To bill an insurance company as an in-network provider, you must first complete this credentialing process.
The first step involves the insurance company verifying that you meet their specific requirements to join their in-network provider panel. This typically includes reviewing your education, training, and professional experience.
Once your practice or organization is credentialed with an insurance company, you'll be able to bill them directly. Additionally, many insurance companies offer providers added incentives, such as:
At Ambit, we streamline the credentialing process, helping you complete applications twice as fast for Medicare, Medicaid, Aetna, Cigna, UnitedHealthcare, TRICARE, and nearly any other provider. Below are just a few of the services we provide on your behalf during the credentialing process.
We ensure that your practice or group has a diverse, popular, and effective mix of in-network payers. Our credentialing team brings extensive experience in enrolling physicians with Medicare, all Medicaid Managed Care plans, and a wide range of commercial payers. We proactively contact each payer on your shortlist to confirm accurate timelines and open panel availability, making the enrollment process as smooth as possible.
We provide you with a comprehensive checklist of all the required information and documents needed to submit your applications. Once we receive your details, our Enrollment team promptly files the necessary contract applications, ensuring a flawless submission from the start, thanks to our extensive experience. Due to our accuracy in first-time application submissions, we take pride in achieving some of the shortest turnaround times for securing contracts.
Our team follows up on the submitted application every two weeks to confirm it has been received, processed, and is in the payer's system. We also ensure that no additional information is being requested and that everything is progressing smoothly. We continue these regular follow-ups until the contract is finalized and delivered to your physical location.
Payers like UHC, Aetna, and BCBS sometimes have closed panels for labs in certain regions. When this occurs, we prepare a detailed appeal highlighting the unique aspects of your services, including specialized offerings and your commitment to exceptional patient care in the area. These details are integrated into your business plan and submitted to senior provider representatives at the payer. While overturning closed panel decisions can be challenging, we have achieved a 35% success rate.
This service is designed for providers who choose to remain out-of-network with certain payers, or those who are forced to stay out-of-network due to closed panels. Our team assists with out-of-network enrollments, NPI registrations on the payer's website, and other necessary steps to ensure your medical practice is in the payer's system, allowing you to start receiving out-of-network payments.
We assist with both basic and complex demographic changes, including updating new TAX IDs with all payers in your mix, changing addresses, bank accounts, and more. Additionally, we facilitate the setup of all ERA and EFT enrollments.
For larger healthcare facilities with multiple providers, precise provider database management is crucial. We oversee and maintain all credentialing data for your providers and physicians through our specialized credentialing portal. This comprehensive, transparent, and HIPAA-compliant tool is designed to ensure your database is managed with the highest level of efficiency and accuracy.
In today's healthcare environment, maintaining up-to-date PECOS and CAQH profiles is essential. With major payers increasingly using CAQH for credentialing and enrolling medical providers, we ensure that your CAQH and PECOS profiles are consistently updated, accurate, and compliant.





When deciding which insurance companies to credential with, it's important to consider the major national plans, such as:
However, it's equally important to identify local insurance companies that could benefit your practice. To do this, consider asking colleagues or other practices in your area which local insurers are most valuable for your patient base.
When you work with Ambit, we conduct thorough network research to ensure your practice or group contracts with the most diverse, popular, and effective insurance providers. We assess various factors, including top payers and your budget, and follow up with you until we get your approval to move forward.
Setting up a private practice often comes with confusion surrounding insurance credentialing and billing third-party networks for services.
The first step in establishing your revenue cycle is to apply for credentialing and secure participating provider contracts with your selected insurance companies. While this process can be complex, Ambit takes on this burden for you. We offer guidance and industry expertise to streamline setting up your new practice's revenue cycle.
Credentialing for government health programs like Medicare, Medicaid, and Tricare follows a different process. These programs require standardized forms that must be accurately completed and submitted to the appropriate intermediary managing administrative duties for your region.
At Ambit, we are well-versed in the strict enrollment standards of these programs. We handle the detailed enrollment process, minimizing the risk of application denial.
If you're wondering how to get credentialed with insurance companies, it's important to understand that the process can take several months, and some insurers may not be accepting new providers. This is where outsourcing the process can be highly beneficial. We offer extensive research and expertise to ensure compliance with each payer's requirements, including:
Many insurance companies split the credentialing process into two stages: credentialing and contracting.
We assist you in submitting participation requests to your chosen health plans using their specified credentialing applications. After receiving your application, the insurance company conducts a thorough verification process, followed by review by their credentialing committee. This phase can take up to 90 days.
Although this phase may seem lengthy, your dedicated Ambit account manager will keep you updated with real-time progress reports, either weekly or daily.
Once your credentialing application is approved, the second phase, contracting, begins. During this stage, the insurance network extends a contract for participation. We support you through the credentialing phase and assist with contract negotiations before you sign, including:
After signing the agreement, you will receive an effective date and provider number, allowing you to begin billing and receiving in-network reimbursements.
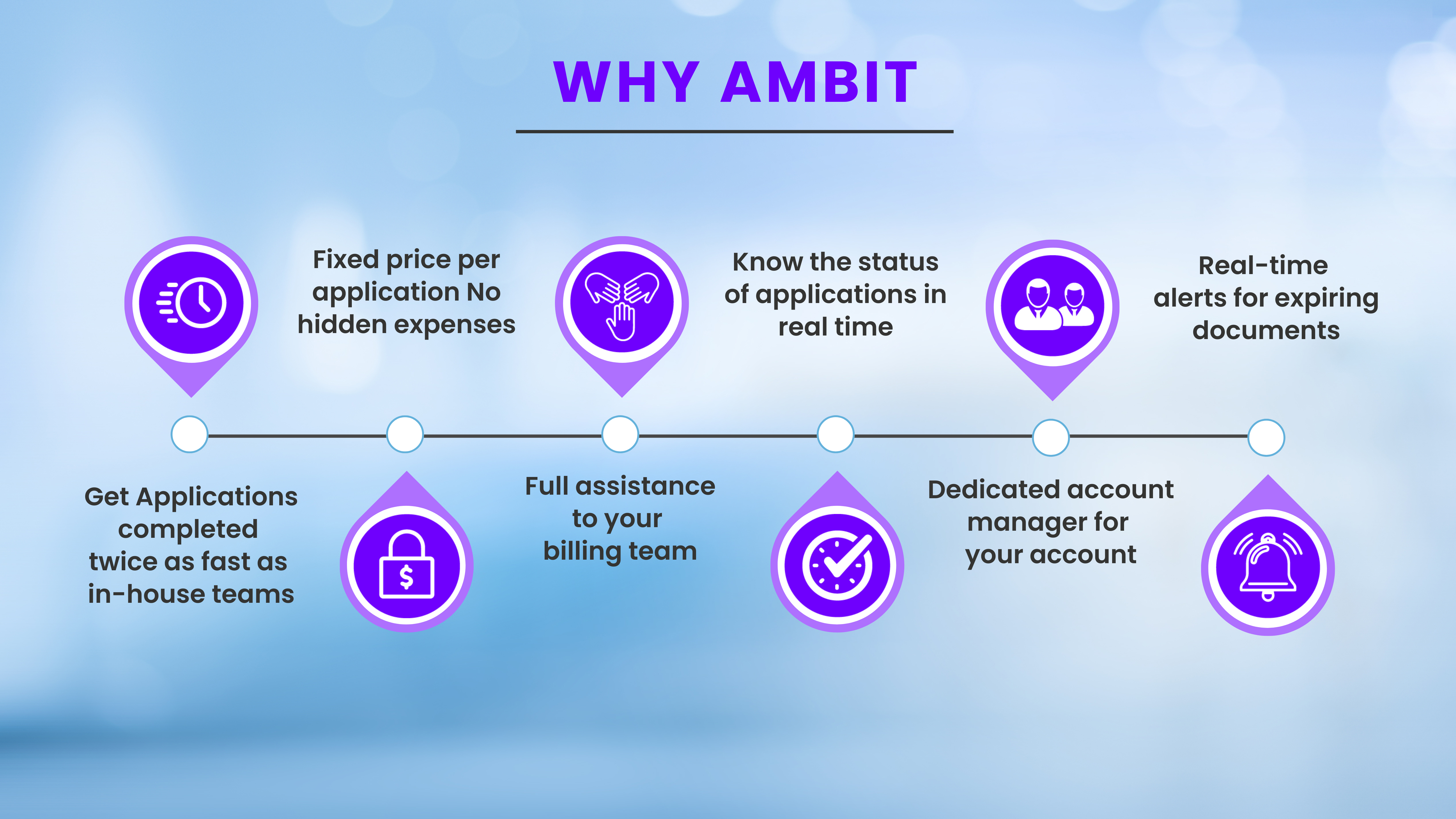
Since 2012, Ambit has partnered with healthcare practices and organizations across the U.S., delivering exceptional credentialing and enrollment services. If you need timely assistance with the credentialing process, we ensure a smooth and efficient experience for both credentialing and contracting.
Countless healthcare organizations trust Ambit because we tailor our medical billing services to meet each client's unique needs. Whether you require consulting or direct action, explore our services by contacting us online or giving us a call at (706) 534 8944 .
Concerned about a growing backlog of claims and approaching deadlines?
We can assist with those as well. Request a free, no-obligation quote for enrolling your providers.




Transparency is essential. Our comprehensive online tool provides a clear view of the entire workflow, application status, detailed reports, and secure, HIPAA-compliant document storage, along with crucial insights into your payer network. By delivering accurate, real-time information to everyone involved in the credentialing process, we've helped leading medical providers reach new levels of transparency and efficiency in payer enrollment. Provider engagement is enhanced with timely information, and expectations are consistently exceeded with clear answers to questions and accurate estimates regarding credentialing costs.
Credentialing is the process of verifying a healthcare provider's qualifications, including licenses, certifications, and professional background. Insurance companies, hospitals, and healthcare organizations require credentialing to ensure providers meet their standards for patient care and reimbursement.
Credentialing is essential for providers to participate in insurance networks and get reimbursed for their services. It ensures that providers meet the required standards of care, which protects patients and maintains the integrity of healthcare services.
The credentialing process typically takes between 60 and 120 days. Timelines vary based on the insurance company and the completeness of the provider's application. Delays can occur due to missing documentation or complex verification processes.
Credentialing typically requires state licenses, DEA certificates, malpractice insurance, board certifications, and a detailed CV. Additional documents may include hospital privileges, proof of residency, and NPI numbers, depending on the payer's requirements.
Ambit can help providers explore alternative enrollment options, such as joining additional insurance networks, participating in government programs, or assisting with out-of-network provider enrollment.
Ambit provides continuous support for enrolled providers, including help with billing, credentialing, and other administrative tasks.
The cost of Ambit's services varies based on the provider's needs, volume, and the payers they are enrolling with. For detailed pricing information, please contact Ambit.
If a provider's enrollment application is denied, Ambit will collaborate with the provider to determine the cause of the denial and create a plan to resolve any issues. In some cases, the provider may need to reapply; in other instances, we may assist with enrolling with a different payer, especially if the current panel is closed or not accepting new enrollments for that specialty.
The documents needed for provider enrollment can vary by payer and provider specialty. Typically, providers must submit copies of their professional licenses, malpractice insurance, NPI, and other relevant documentation. Ambit provides comprehensive support to assist providers in preparing for the enrollment process.
By clicking submit, you agree to our Terms and Conditions and Privacy Policy.
By providing a telephone number and submitting the form, you are consenting to be contacted by SMS text message. Message and data rates may apply. Reply STOP to opt out of further messaging.