BEV is a vital component of the RCM cycle. We ensure that your patients' plans cover the procedure you’re about to perform, which helps prevent eligibility-related denials and boosts revenue by at least 7-10%.
We thoroughly review claims to maximize reimbursements while avoiding over-coding, which generally increases client revenue by 10-20%. We boast a near 100% success rate for first-attempt HCFA and UB clearinghouse claims, including WC (workers' compensation) and NF (No Fault) claims. Additionally, we keep up-to-date with the latest coding updates.
Insurance claim denials are a common challenge, making AR follow-up a crucial aspect of any billing workflow. Effective accounts receivable follow-up ensures prompt resolution of rejections and denials. At Ambit, we allocate substantial resources to our AR follow-up team to ensure that a high volume of submitted claims is promptly addressed, allowing for swift action and reworking of denials.
We ensure that your accounts receivable face minimal denials. Our experts are highly skilled in overturning a wide range of denial types, including medical necessity denials, exhausted benefits, requests for additional documentation, coding issues, patient benefit problems, prior authorization challenges, and EDI issues. Our team excels at resolving these issues through timely and effective follow-up and comprehensive appeals.
We have a dedicated appeals and reconsiderations team that collaborates closely with the AR team. This team utilizes both standard and customizable appeal formats for every type of denial. Thorough and timely appeals, containing the correct information, can significantly impact the successful overturning of even the most complex denials.
We ensure that all your EOBs (Explanation of Benefits) and ERAs (Electronic Remittance Advices) are posted and reconciled daily to provide your staff with an accurate end-of-day statement and track average revenue growth. Our two-tier quality system guarantees that every posting undergoes both a level 1 and a level 2 review before the final reconciliation report is generated.
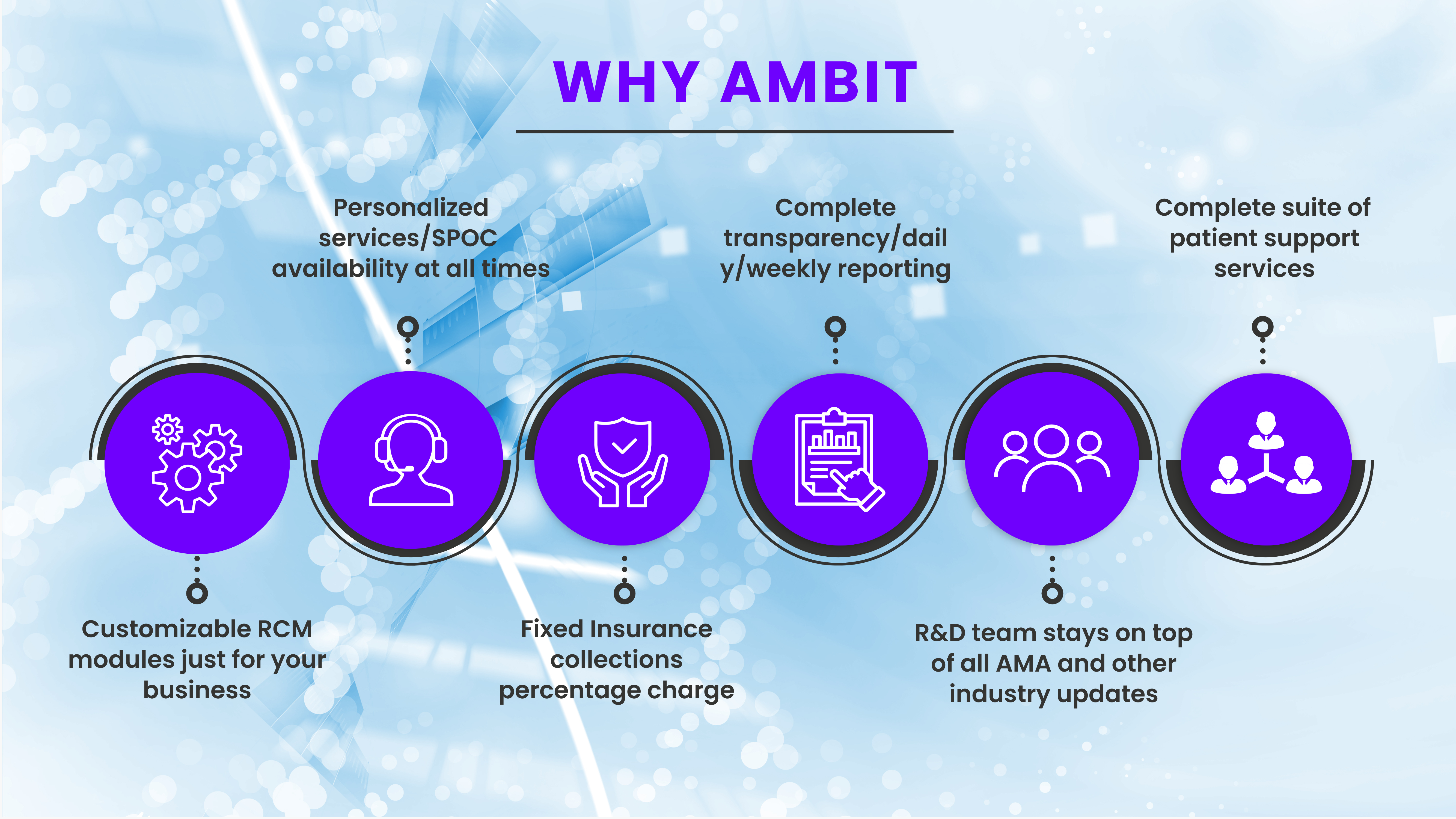
We maintain a high level of transparency in our billing workflow with clients. We provide clients with access to the billing team's workflow logins for complete visibility and share all reports on a weekly basis. Additionally, we schedule monthly REM sessions to present a clear roadmap, review all aging and revenue reports, and outline our strategies for enhancing collections and driving revenue growth in the upcoming quarter.
Every practice, laboratory, or healthcare institution dealing with insurance claims faces the challenge of aged AR or stuck AR. These are insurance denials, rejections, and claims with missing information that remain unresolved, often due to being short-staffed, lack of effort or resources from your billing company, or simply being overwhelmed with administrative tasks, causing billing and aged AR to be neglected.
This is money left on the table—funds that could have been collected to boost your bottom line.
We offer a straightforward solution. There's no need to fire your biller or billing team, change software, or incur additional costs to hire us. Just hand over that aged AR to us, and we’ll work to collect those unresolved denials and rejections. We only get paid when you recover that lost or aged AR. It's that simple.
With 10+ years of experience in RCM, working with over 300 practices nationwide and a team of more than 120 skilled billers, we have mastered one of the most critical aspects of RCM: Denial Management.
This is money left on the table—funds that could have been collected to boost your bottom line.
Each time we took on a practice's billing, we set a goal to reduce the denial rate by 18-20% within the first quarter. We are proud to say we’ve consistently met this target. This success led to the creation of our credentialing and enrollment division, as we understand that effective denial reduction is closely tied to proper credentialing.

Hospitals often have millions in aged or unresolved accounts receivable that they’ve written off. Let our experts in aged AR come in to strategize and reclaim what is rightfully yours.


Outsourcing your medical billing to Ambit Global Solution can lead to faster claim processing, reduced overhead costs, fewer errors, and improved cash flow. Our expertise allows your practice to focus more on patient care rather than administrative tasks.
We understand that every practice has unique needs. We work closely with each client to develop a tailored billing solution that aligns with their specific requirements, ensuring the best possible financial outcomes.
We use advanced billing software and employ a team of certified medical billers who are experienced in coding and billing practices. Our multi-step quality control process ensures that every claim is thoroughly reviewed for accuracy before submission.
Yes, Ambit Global Solution has expertise in billing for a wide range of medical specialties, including but not limited to, general practice, cardiology, dermatology, orthopedics, and mental health services.
Our dedicated denial management team investigates every denial, corrects any errors, and resubmits claims promptly. We also provide detailed reports and recommendations to help prevent future denials.
Our onboarding process is streamlined and efficient. We start with an initial consultation to understand your needs, followed by system setup, data migration, and staff training. Our team is with you every step of the way to ensure a smooth transition.
Getting started is easy! Simply contact us through our website or call our customer service team to schedule a free consultation. We'll assess your needs and provide a customized proposal for our services.
We provide detailed, transparent reports that cover all aspects of your billing cycle, including claim status, accounts receivable, payment trends, and denial analysis. These reports are available on-demand through our secure client portal.
Yes, we understand that medical practices often need support beyond regular business hours. We offer extended support hours and have a dedicated team available to address urgent issues.
Ambit Global Solution stands out due to our commitment to personalized service, industry expertise, and advanced technology. We are dedicated to improving our clients' financial performance while maintaining the highest standards of accuracy and compliance.
By clicking submit, you agree to our Terms and Conditions and Privacy Policy.
By providing a telephone number and submitting the form, you are consenting to be contacted by SMS text message. Message and data rates may apply. Reply STOP to opt out of further messaging.